The holidays are a time for connection, celebration, and reflection, but for those in recovery, this season...
Addiction
read more
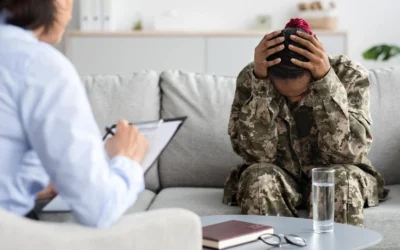
Veterans Day: PTSD Treatment and Addiction Programs with CRC
On November 11, we honor and remember our veterans for their sacrifices and acknowledge the challenges they...
Signs You May Need Mental Health and Addiction Treatment
When mental health challenges and addiction overlap, it can be challenging to know when a dual diagnosis...
Link Between Mental Health and Substance Use Disorder (SUD) – Depression Awareness Month
October is Depression Awareness Month, a critical time to highlight the important connection between mental...
Trauma in Addiction Recovery: The Importance of Trauma-Informed Care
Trauma plays a significant role in the development of addiction. Many individuals struggling with substance...
The Role of Family Therapy in Addiction Recovery
Addiction is a family disease that affects not only the person struggling but also their loved ones. Because...