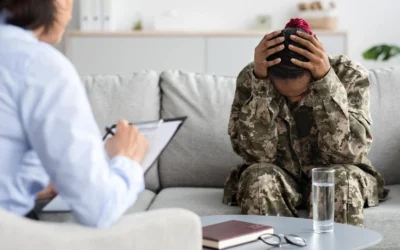
June is PTSD Awareness Month, a time to raise awareness about the effects of trauma and highlight effective...
Veterans Health
read more
Veterans Day: PTSD Treatment and Addiction Programs with CRC
On November 11, we honor and remember our veterans for their sacrifices and acknowledge the challenges they...
What is Cocaine? Facts, Prevention, and the Path to Recovery
Cocaine has long been a potent and dangerous drug, contributing to significant public health issues around...
Dual Diagnosis Among Veterans and the Importance of Treatment for Lasting Recovery
For many veterans, the transition from military to civilian life is filled with challenges that can deeply...
Signs of Cocaine Addiction: Recognizing the Signs and Supporting the Path to Recovery
Cocaine addiction continues to be one of the most serious substance use issues in the United States. Despite...
Helping Veterans Overcoming Alcoholism and Addiction
As we come together to celebrate Independence Day, we pay tribute to the bravery and sacrifices of our...